84% of women say before birth that they intended to exclusively breastfeed; Yet studies have found that only 53% of women reported that they were exclusively breastfeeding after birth.
So why is it so difficult for women to breastfeed in Ireland?
Inspired by Lord Mayor Hazel Chu post looking for suggestions to improve breastfeeding support services, four mothers banded together to find out.

Deborah Byrne and Felicienne Rahill (Research), Lucia Prihodova (Analysis) and Megan Etherton (Design & Illustration) were, inspired by their own experiences of breastfeeding support within Irish Maternity units. They recently launched a social media campaign, a petition and the publishing of a report called Bainne Beatha, with the aim of improving Irish breastfeeding support services. They are running this campaign in their spare time, without funding or affiliations.
In response to the Lord Mayor’s question, Deborah decided to create a questionnaire in order to compile friends’ responses. The questionnaire spread organically through social media and received 145 unique responses. When the women began combing through the responses together, they quickly realised that responses indicated that Irish Maternity Hospitals have not yet fully implemented the National Maternity Strategy 2016 - 2026, the HSE Breastfeeding Action Plan 2016 - 2021, nor do they consistently practise WHO/Unicef Breastfeeding Guidelines.
The National Maternity Strategy aimed to map out the future for maternity and neonatal care, to ensure that it would be safe, standardised, of high-quality and offer a better experience and more choice to women and their families. It pledged that across all pathways, care would be woman-centred and provided by a multidisciplinary team.
This failure has led to Bainne Beatha: a social media campaign, a petition to the minister, and the publishing of a report of the findings with the aim of achieving the following:
- They would like their breastfeeding stories to be heard.
- They would like their stories and this petition to mobilise those with the power to enable full implementation of these policies to do so.
The petition commenced on January 28th, and has garnered significant interest and support. The intention is to send the petition to the Minister for Health on February 26th, along with the Bainne Beatha report, with the objective of securing a guarantee that the National Maternity Strategy and the HSE Breastfeeding Action Plan are fully implemented in Ireland.

Report summary:
- 9 in 10 mothers said that feeding did not go as planned and each experienced an average of three challenges which affected their ability to breastfeed.
- 37% of women reported that midwives seemed pro-breastfeeding but were too busy and overworked to provide the assistance needed.
- 27% of women reported lack of assistance in the hours post delivery.
- 29% of women said they received conflicting advice from hospital staff about how to breastfeed.
- Qualitative data indicated that some physiological challenges were missed, and staff lacked up-to-date knowledge on breastfeeding.
- Only 1 in 3 women felt fully supported in implementing their feeding goals.
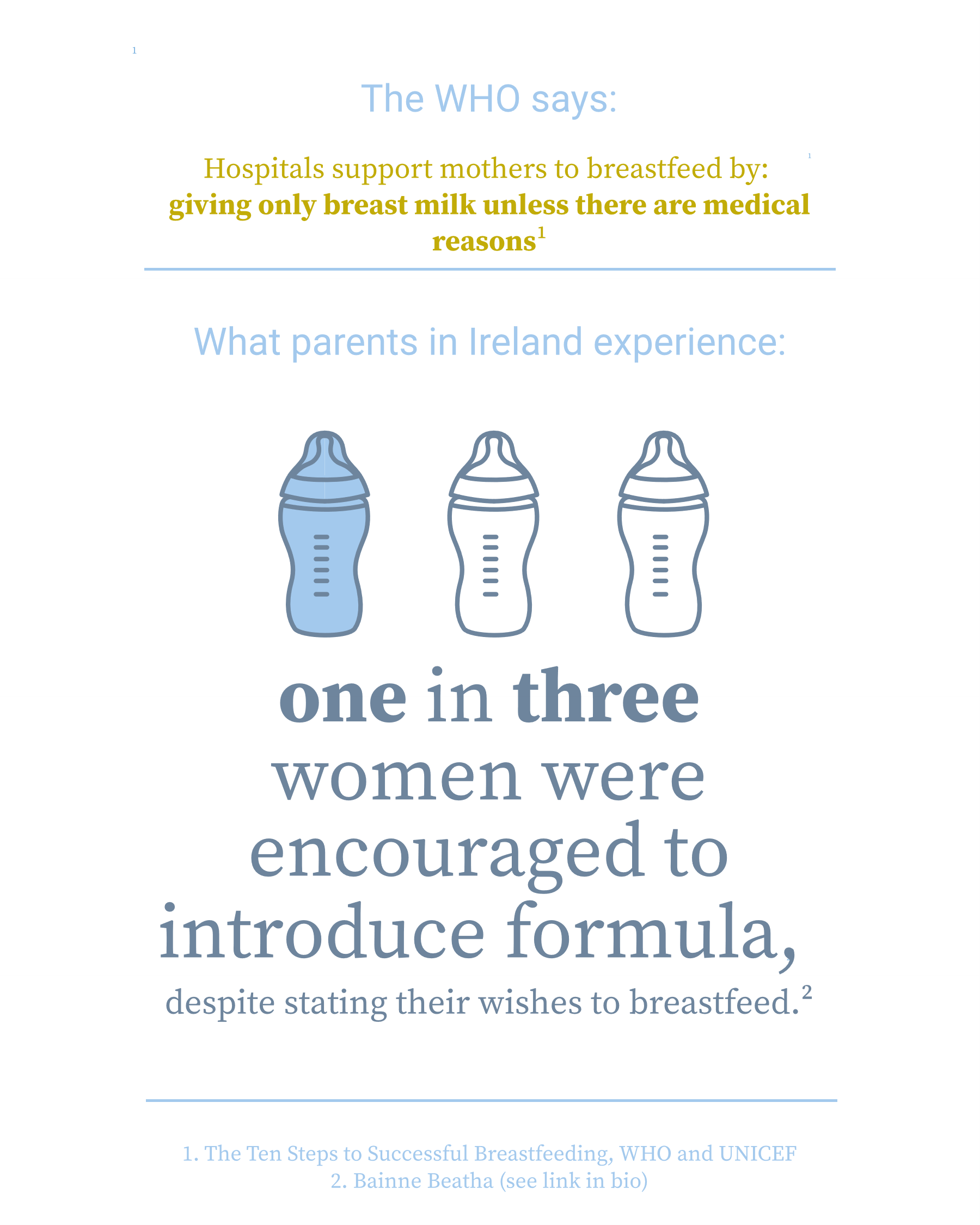
- 1 in 3 mothers were encouraged to give their babies formula, despite expressing wishes to breastfeed. No mothers reported the availability of human donor milk in lieu of formula.
- Some mothers felt there was a disconnect between recommending breastfeeding and investing time and effort in helping mothers to get it right and felt that some staff preferred the convenience of formula as evidenced by the formula trolley.
- Others commented that rather than taking the time to assist in latching, mothers were encouraged to pump as a quick fix solution.
- 1 in 3 mothers felt their antenatal classes didn’t provide enough information on breastfeeding.
- 60% of women spent an average of €440 to get help with breastfeeding challenges through the hiring of private lactation consultants, breast pumps, tongue tie procedures and other feeding related expenses.
- Only 1 in 4 mothers reached their feeding goals at the hospital and did not require any further support with breastfeeding after discharge.
What the report calls for:
- Dedicated International Board Certified Lactation Consultants (IBCLC) who are at specialist competency level (as per HSE Competence Framework for Breastfeeding Support, 2015) available 24 hours per day in the maternity hospitals to assist mothers to establish breastfeeding.
- Intensive feeding support in the immediate hours after baby’s birth.
- Early intervention when challenges with breastfeeding occur.
- Mothers only discharged from lactation service once breastfeeding is fully established.
- Facilitate regular training on breastfeeding for midwives and IBCLCs in line with up-to date evidence-based practice.
- Access to in-depth, evidence-based antenatal classes on breastfeeding for all mothers.
- Review of the policies on promotion and distribution of formula in maternity wards in line with international practice.
- The National Maternity Experience Survey to expand questions on feeding to provide greater detail on breastfeeding rates and breastfeeding experiences in maternity care.
- Annual audit of service users (mothers) to be carried out by the maternity hospitals to ascertain their experience of breastfeeding support from service providers.
- Annual national campaign to inform and promote breastfeeding in Irish society.
How you can help:
Sign their petition here to get these demands heard.
Join in their social media campaigns on Twitter @bainnebeatha, Facebook @bainnebeatha and Instagram @bainnebeatha.
Email them at mailforbainnebeatha[at]gmail.com with any feedback, comments, questions or suggestions you may have for the campaign!